Surgical techniques have improved to be minimally invasive and less painful.
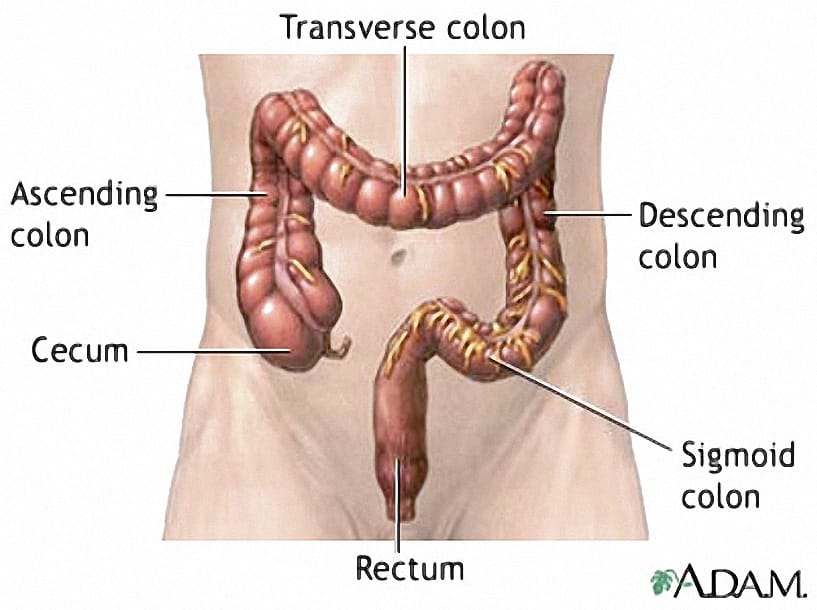
Most bowel cancers occur in the final part of the large bowel before the anus, called the rectum. Treatment of rectal cancer can include medication in the form of chemotherapy, radiation therapy and/or surgery. In surgery, the rectum together with the ‘cushion’ of tissue containing lymph nodes and blood vessels surrounding the rectum, called the mesorectal, must be removed (see image below).
This is called Total Mesorectal Excision (TME) and is the gold standard approach to rectal cancer surgery as it has been shown to reduce the risk of cancer coming back and people can live longer after being cured of bowel cancer. The way in which surgeons perform rectal cancer surgery has undergone significant advances over the last few decades.
The development of more minimally invasive approaches including ‘keyhole’ (laparoscopic) and robotic surgery has enabled surgeons to remove the rectal cancer through smaller cuts. These less invasive techniques have been associated with less pain after surgery, faster recovery and shorter stay in hospital. For early rectal cancers, techniques that remove the growth through the anus have also been devised, including Transanal Endoscopic Microsurgery (TEM) and Transanal Minimally Invasive Surgery (TAMIS).
A combination of these methods has been applied to advanced rectal tumours and led to the development of the latest technique called transanal Total Mesorectal Excision (taTME).